By: Chad Wooters
Getting Started in Dental Sleep Medicine Can Be Simple
It doesn’t have to be complicated, it just doesn’t. The best way to start offering a new service in your dental practice is to start simple. Once you see successful patient outcomes and understand how you can make money as a business, you can “invite complexity” to your sleep program. In this article, we will explore the fundamental concepts a team must understand to get started in dental sleep medicine.
There are many factors to consider when you are starting your sleep program. If you want to explore some of the factors, read the “Getting Started in Dental Sleep Medicine” article.

What are the fundamentals of dental sleep medicine?
The Fundamentals of DSM
There are four fundamentals to get started in Dental Sleep Medicine. These four ideas will allow you and your dental team to start making progress in helping patients with this life-saving treatment. The four fundamentals are:
Team Structure
Learn the Basic Structure of a Sleep Business Along With Key Questions and Roles That Need Filled
Patient Communication
Learn the Key Components of Sleep and How to Best Connect With Patients
The Impact of OSA
Explore the True Impact Sleep Apnea is Having in and on Your Patients Lives
Screening Patients and Next Steps
Understand Screening Patients for an Airway Concern and Start the Path to Treatment
Let's explore these ideas in more detail.
Overview
Team Structure
Dental Sleep Medicine (DSM) is often called a “different type of dentistry.” This doesn’t mean that you have to stop what you are doing in your dental practice. But you may need to shift your perspective on how your program runs.

In most dental practices, the highest earning procedures are those procedures that the doctor performs. These could be implants, reconstructive surgeries, trauma cases and others; in most of these treatments, the doctor’s time is heavily taxed.
In DSM, the requirement on the doctor’s time can be minimal when the team is doing a majority of the work. The dentist should be spending between 20 – 40 minutes with each sleep patient unless complications arise. Since DSM is a different type of dentistry it can require a slightly different set of roles.
What are the roles needed in a sleep program?
Let’s start with hygiene. Hygienists, you are commonly referred to as the lifeblood of a restorative practice and your sleep program is no exception. You are often considered to be a “trusted advisor” to your patient since you see them so frequently. You will play a role in the screening conversation and the communication to the patient about the things that are concerning to you about their airway.
Next is the dental assistant! Dental Assistants, most often you are the “Sleep Champion”. Sometimes this role is referred to as the “Back Office Sleep Champion”. You are the one who will guide the patient through their testing process and entire treatment plan. You will be the point person for sleep in your practice. There is typically only one Sleep Champion in a practice, so not every dental assistant is responsible to lead the patient.
Third is the front office team. Front Office, you are “The Closer” or also referred to as “Front Office Sleep Champion”. You are the one who comes in and scores the touchdown. You help make things happen for the patient, administer the home sleep study and present the treatment plan for oral appliance therapy. Your role makes all the team’s hard work turn into revenue for the practice.
Last (but certainly not least) is the doctor. Doctors, you are the “Enabling Leader.” You are the one who assigns these roles, calling your team up, and being the foundation the team leans on when they need help. You set the tone of your program and equip your team for success in their new roles.
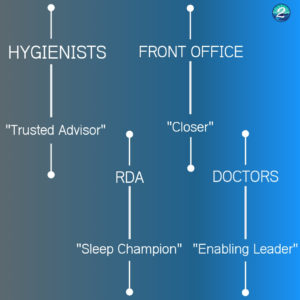
When you start treating sleep in your practice the doctor may have to spend more time on each case, but as the team grows and the program is developed you will see how each person can take more of their role and create a simple system to help patients within your practice.
Note: Dental Sleep Medicine is not a one-size-fits-all type of program for dental teams. The above roles are the typical roles that we find in a successful dental sleep medicine program, but can be adjusted with your unique practice.
Dental sleep medicine should fit inside of your existing dental practice, without breaking what makes your dental practice work.
Patient Communication
Working with patients who have an airway issue or sleep disorder requires a different set of tools than normal dentistry. When a patient comes into your practice and needs dental work, their perceived need for treatment is typically more obvious than with sleep apnea. When a patient is in pain and you can show them an image using an X-ray or CBCT image, they are more prone to understand a problem that they can see.
When we start talking about the airway and sleep, we are talking about an almost “invisible” condition. Here are some obstacles that hinder effective patient communication in dental sleep medicine:
- Snoring is considered normal in our society
- Being tired is a common way of life for many people
- Patients think instantly fall asleep at night is a sign of sleeping well
- Fatigue is thought to be a symptom of overworking and nutrition, not a sleep problem
- Every symptom has some excuse (or more!)

When you talk to patients you need to learn a set of soft skills that we call “Hero Positioning.”
Hero Positioning is when we connect to what really matters to our patient using active listening, understanding the patient’s aspirational identity, and helping the patient recognize that their symptoms are the “villain” in the story of their health.
For more information on the hero versus villain positioning, check out our article on “Building a Storybrand” by Donald Miller.
The Impact of OSA
Sleep apnea and sleep related breathing disorders have a huge and lasting impact on people who go untreated. This is slightly different from everyday dentistry as Dr. Greg Manning has said, “Nobody ever died of missing or crowded teeth, but people die every day from sleep apnea.”
1. It allows our teams to connect the purpose of treating this life-threatening condition
2. It provides a deeper understanding of how we can communicate with patients and identify who is at risk
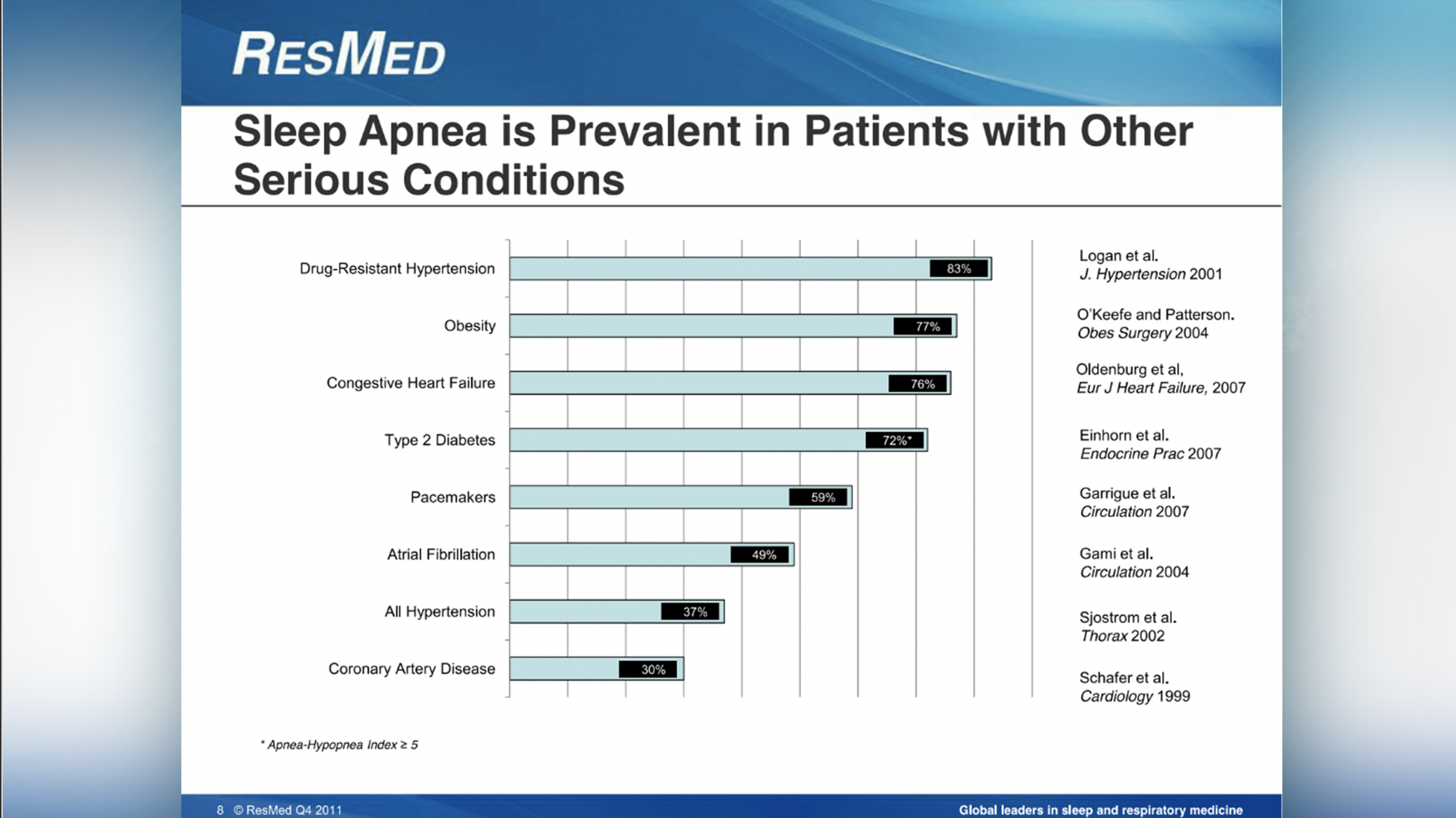
Patient’s who have undiagnosed OSA have one or multiple of the complications in the image to the right.
Can you think of a patient who suffers from:
- Drug-resistant Hypertension
- Type 2 Diabetes
- Obesity
- Hypertension
Look at this study by Resmed below. These patients are paying with their lives every day that they go undiagnosed. Having our team understand why we are doing this is critical for success in our program and patient communication.
Screening Patients and Next Steps
The final fundamental concept is screening our patients and moving forward in helping them with the next steps in discovering if they have a problem. Working in dental sleep medicine there are 3 phases of the process.

In this process, getting patients diagnosed and back to our dental practice when they are able to be treated with a mandibular advancement device can seem complicated.
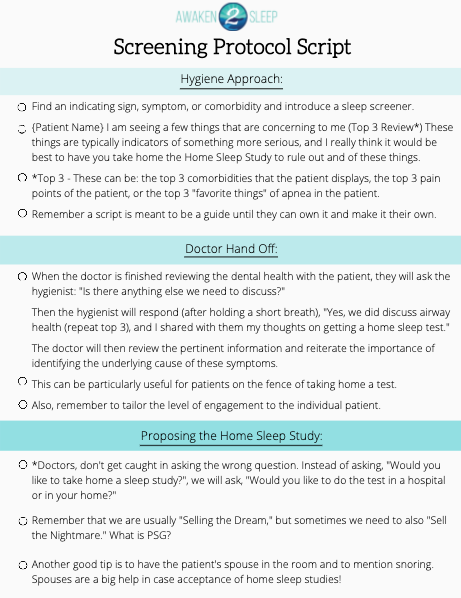
The most difficult part of the process isn’t finding patients who are at risk; it’s helping them get a sleep test that is diagnostic so that they can learn what treatment is best for them! We recommend a simple protocol that allows a team to connect to a patient and help them with that test. We call this script the “3 Favorite Things” Protocol.
After the patient has been screened, their next step in the process is to complete a sleep study. Depending on the purpose of what we’re testing for, they can do an in-lab study called a Polysomnogram or they can do an at-home study called a Home Sleep Test. In most states, dentists can own and operate their own home sleep studies. Please verify with your dental board guidelines for any restrictions or requirements within your state.
Once the patient has received a test we need to verify that a Board-Certified Sleep Physician has interpreted that sleep study.
IMPORTANT: A dentist CANNOT interpret a home sleep study, as it is outside of the dental scope of practice to read and interpret the results of a sleep study. We recommend that you find a company that can help connect you with a Board-Certified Physician in your state.
If you need an interpreting provider click here to learn more about our interpretation services.
How Do I Teach My Team the Fundamentals?
A common question for practices is: “How do we teach our team members the fundamentals of DSM?”
These concepts are taught in the “Dental Sleep Medicine Implementation” Course.
The course includes:
- Admission for 1 Dr. + 4 Team Members
- 14 CEs for Each Attendee
Course Bounses:
- Workbooks
- Over $2000 in savings from the appliance manufacturers
- Interactive breakout groups with industry experts
- Action plan to help you build your custom systems
Enter Coupon Code: A2S200
Bring your team (up to 4 additional team members) and your doctor (1 doctor) for $597!
Usually $797!