How To: Get Started in Dental Sleep Medicine
What is Dental Sleep Medicine?
Dental Sleep Medicine is defined by the American Academy of Dental Sleep Medicine.
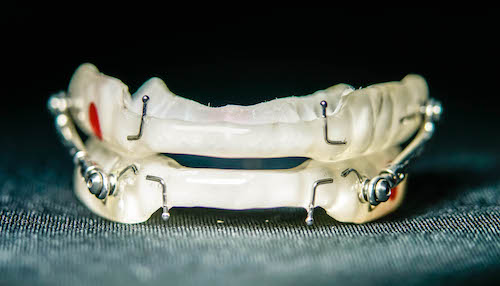
“Dental sleep medicine is an area of dental practice that focuses on the use of oral appliance therapy to treat sleep-disordered breathing, including snoring and obstructive sleep apnea (OSA).”
Simply put, dental sleep medicine is when a dentist is involved in treating sleep disorders that are due to an obstruction of an airway. An obstruction is some physical collapse of the airway. This could be caused by the tongue falling back into the airway or soft tissue congestion that causes a blockage.
The device called an “oral appliance” or sometimes referred to as a “mandibular advancement device” is a custom fit device that is made for a specific patient and pulls the mandible (lower jaw) forward to help pull the tongue forward and hold the airway open.

How does a Dental Practice Get Started in Dental Sleep Medicine?
It is important to recognize that dental practices are made of individual people, who are all different. They each have their own culture and systems and each one is unique.
There is no one-size-fits-all strategy for all dental practices.
However, there are similar components that each practice can consider in getting started. Some of these components are:
Team Training Programs
What Dental Sleep Medicine Training is Best?
Unfortunately, this is the wrong question. Each practice has to consider which training is right for you. The correct question is:
What Dental Sleep Medicine Training is Best for Us?
Here are some of the ways to determine what training mode is best for you. Use the questions below to guide your decision
Considerations:
- How many people on the team?
- How does your team respond to instruction?
- Do they own ideas and self start or do they require accountability and hand-holding?
- Will they pay attention and retain digital or group content?
- Do you want a one-time training or an ongoing arrangement?
For further guidance on determining which training program is best for your team, you can schedule a call with a sleep coach below.
Coaching Programs
The same issues that come with determining the right fit for a training program also affect coaching programs. You need to find the coaching that works best for you. Here are some of the considerations for coaching programs that you should ask before committing to a coaching program.
Considerations:- What does the company mean by “coaching?”
- How many times am I going to talk to my coach?
- Is coaching live or digital?
- If the coaching is digital, does it include video or just phone calls?
- What is the financial commitment and the minimum time commitment?
- What are the results of this coaching program?
- With this coaching program, what else will I need to have/purchase to have a successful program?
Diagnostic Equipment and Diagnostic Services for Dental Sleep Medicine
Can a dentist own or operate a home sleep study?
Dentists in most states in the US can own and operate Home Sleep Testing Equipment. There are a few states in which you cannot own and operate equipment. Since the ADA’s release of its position on this topic in 2017, state boards have predominantly supported their statement.
Click Here to View the ADA Position Statement
That being said, dentists cannot diagnose obstructive sleep apnea (OSA) in patients.
Diagnosing OSA remains and/ or interpreting the results of a home sleep study remain outside the scope of practice for dentists and require a Board-Certified Sleep Physician’s interpretation. The guidelines from the ADA and most dental boards share requirements that treatment of patients with Sleep-Related Breathing Disorders with Oral Appliance Therapy must be done under the recommendation of a physician.
There are two ways to get a patient tested for obstructive sleep apnea. They can either do a Polysomnogram (in-lab sleep test) or a Home Sleep Study.
For more information on these two tests please click here.
As it relates to home sleep testing, there are two models that a practice can use:
In-House Home Sleep Testing

- Practices that own and operate HSTs will bill patients themselves for the testing
- You can use HSTs to do a Medical Billing Model or a Fee For Service Model
- Many dental practices charge between $100 and $200 comfortably for HSTs
- Faster workflow and helps increase production
- Requires an “interpretation service.”
3rd-Party Home Sleep Testing

- A dental practice will screen a patient and send documents to a service that will ship a test directly to the patient
- Typically the service will send the report to the referring provider
- Requires a longer workflow
- Lower patient compliance
- Faster workflow and helps increase production
- Sometimes these services will attempt to provide patients with CPAPs even when a dentist refers them to their testing service
Neither model is bad. Some practices are in a position to move forward with an “in-house” model, while others need to build up their program or team before bringing testing “in house”.
Still have questions, talk to a sleep coach for free!
Communication Tools
How we communicate with our teams and patients is critical to our sleep program! Some of the common tools to increase communication are below!
Technology
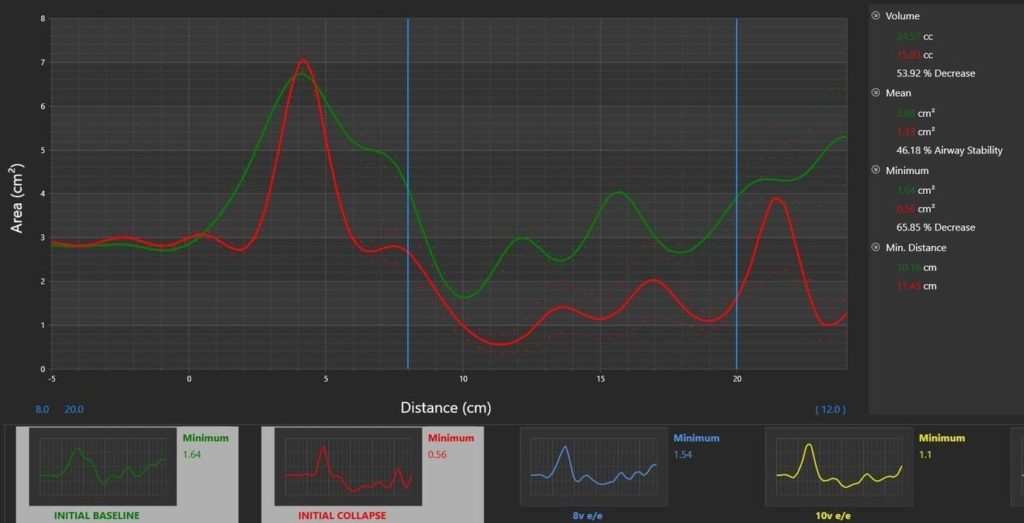
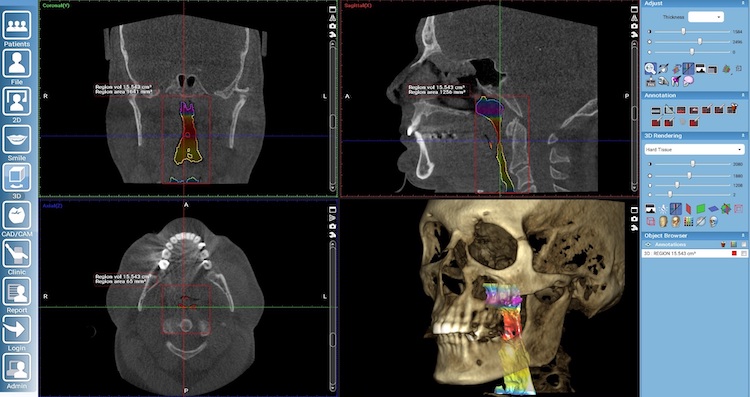
CBCT (Cone Beam Computerized Tomography) Technology
- CBCT (Cone Beam Computerized Tomography) Technology
- CBCT cannot diagnose OSA
- CBCT can create an image that demonstrates constriction of the airway
- CBCT can be used to start a screening conversation
- CBCT can be used for the creation of certain Mandibular Advancement Devices such as the SICAT Optisleep
Pulse Oximetry
- An inexpensive tool to help provide screening evidence of oxygen desaturations indicating the need for further evaluation of the airway and more diagnostic studies
- Cannot diagnose OSA independently
- Can be used to convince patients that there is an issue
- The downside is that it adds potentially unnecessary steps to your workflow

And More! More technology is becoming available all the time. These are just common technologies for patient communication.
DSM Forms
There are so many forms available, here are some of the common ones!
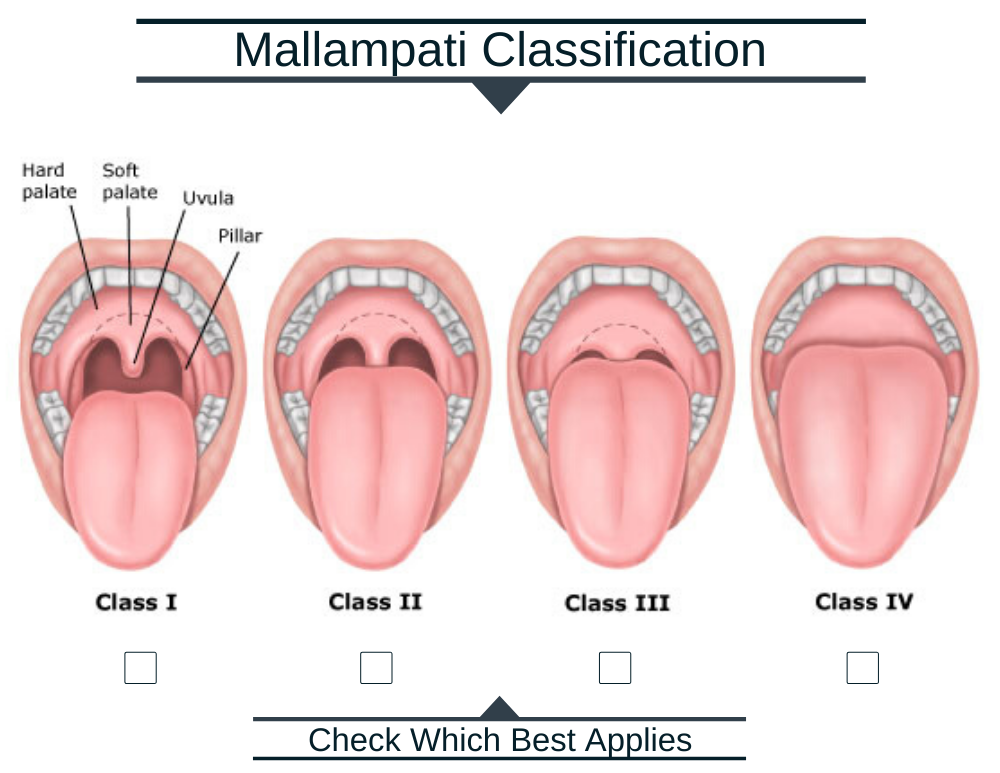
Mallampati
Designed by Dr. Mallampati (anesthesiologist) to evaluate the risk of an obstructed airway while being sedated and/ or during post-op recovery after general anesthesia.
Epworth Sleepiness Scale
Download the Form
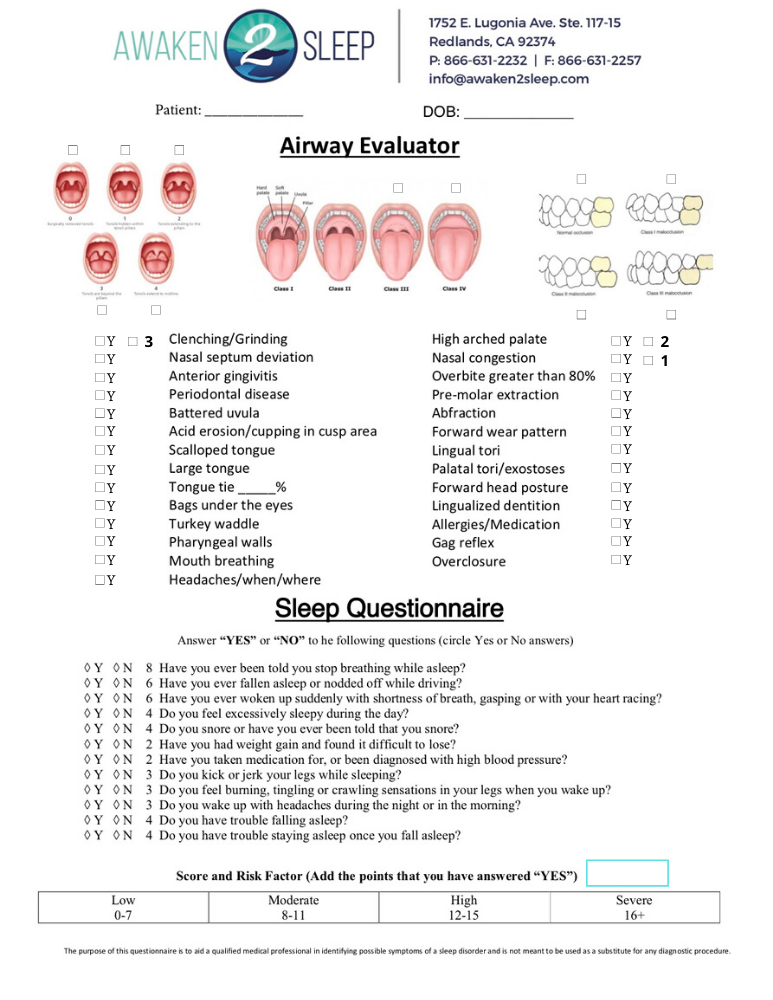
Click Here to DownloadAwaken2Sleep Screener
Comprehensive evaluation that combines the Mallampati, occlusal classification, tonsil size, medical comorbidities, dental comorbidities, and a subjective patient evaluation to communicate comprehensive patient risk for airway obstruction.
Soft Skills
Dental Sleep Medicine is a different type of dentistry, so it requires a different set of skills! Here are some of the skills you should consider!
Patient Friendly Verbiage
Keep the conversation less clinical, most patients don’t understand or relate to clinical verbiage. Use more common words!
Identify Patient Pain Points
Connect with the patient on what is hurting them the most.
"People don't care what you know until they know that you care"
Hero Positioning
Help empower the patient by positioning their pain as a “villain” and give them tools to overcome that villain!
Each category of communication has more details that can be explored in greater depth. As a dental professional, you have a unique opportunity to help save lives by being involved in helping patients with obstructive sleep apnea and treating patients who fit within your scope of practice.
If you are looking to get involved in DSM and want to find out more about the next steps you need to take to get the results you want, use the button below to connect and schedule a call with a sleep coach.