By: Steve Carstensen, DDS
It’s time to pick a movie for tonight. Scrolling Netflix provides hundreds of choices, many sound good, and your partner gives you no help. How do you settle on one?
There are more than 120 oral appliances FDA cleared to treat sleep-related breathing disorders, SRBD. Your patient is waiting for you to recommend one; your team needs to know which prescription form to fill out. How do you choose?
One essay is not enough to work through the entire list, so I’ll focus on the TAP group of devices, let you know about how they were developed, what the science says about effectiveness, and provide some clinical uses that are unique to the Thornton Adjustable Positioner.
Keith Thornton, a third-generation restorative dentist in Dallas, was also a Pankey Faculty member, part of the original group of clinicians who formed the Institute in 1969. In 1989, he taught me about taking care of the whole person, and as the TAP ideas for treating SRBD were developing in the 1990s, there were several of us included in early device use. From the original TAP1 through today’s dreamTAP, every iteration launched by engineer/entrepreneur/clinician Dr. Thornton has been aimed at providing evidence-based therapy for people suffering from poor breathing during sleep due to a collapsing upper airway.
Dentists Are The M.A.D. Doctors!
Because that’s what dentists deal with: a mechanical closing of the upper airway due to pressure changes during sleep, particularly during REM sleep, and especially while supine. If you think about the anatomy in three dimensions, overlay that with muscle tone changes and pressure differentials, and imagine all that in a supine body, it’s not difficult to visualize the pathophysiology of snoring, upper airway resistance, or obstructive sleep apnea.
Keeping that airway open with a mandibular advancement device, MAD, is our part to play in treating OSA. Physicians, thankfully, leave it up to us to use our expertise to choose which MAD.
Protruding the mandible with a TAP relies on anchorage on the maxillary teeth and an active forward pull on the mandible, using teeth (or implants) to overcome gravity, negative pressure in the oropharynx, and the elasticity of the anatomy. It’s as simple, and as complex, as that. Dentists are required to examine the oral structures and function of the movable mandible to ensure compatibility with oral appliance therapy, and to fit and follow-up the MAD. There is no other medical provider trained like dentists to care for patients in all the details needed.
Your Patient's Diagnosis Impacts Your Treatment
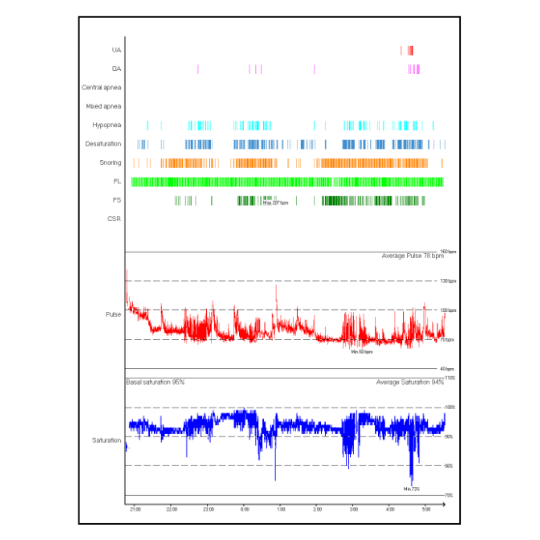
Consider your patient’s diagnosis. What is the nature of the sleep breathing disorder? Are the events primarily apnea or hypopnea? Is there a big difference between supine and non-supine sleep position? Between REM and NREM stages? Each of these details can help you choose the best appliance.
If your patient has a largely supine-dependent SRBD, resisting gravity to keep their jaw forward is paramount. Some MAD designs, like 70-degree dorsals or Herbst, perform poorly in this circumstance unless elastics are used to maintain mouth closure, adding complexity to the therapy. TAP has a secure anterior midline connector that I explain to patients like ‘hanging a coat on a hook.’ MAD with the adjustment strap anchored in the maxillary anterior, such as EMA or Avant, and 90-degree dorsal devices, such as ProSomnus, also require no elastics.

Patients with predominately hypopnea events generally require less protrusion than those with more apnea episodes. Some of those patients may respond very well to nasal airflow improvements, so you can begin with nasal clearing techniques, breathing coaching, and minimal advancement.
The myTAP professional interim MAD is very helpful in this instance because it requires no prescription or lab-manufacturing time and comes with a silicone mouth shield to promote nasal breathing during sleep. Lip-taping can be very helpful if the patient is willing to take that step and the tape can be applied to their face. The myTAP mouth shield is useful for everyone, with modifications to fit around the frenula, for example, simply a matter of trimming using scissors.
If the patient successfully transitions to all nasal breathing, they sometimes maintain enough pressure in the upper airway to reduce the obstruction events to normal and maintain adequate blood oxygen levels. This requires more professional interaction than simply handing the patient a well-fitted MAD, so team members must be trained and systems put in place to evaluate subjective and objective data as SRBD are addressed using nasal breathing improvements as the primary therapy. The myTAP is useful to bridge the gap between diagnosis and patient self-efficacy and is handy for patients to keep ready in case they start mouth-breathing or suffer setbacks in upper airway performance.
Most people diagnosed with SRBD have their worst breathing during REM sleep due to inhibition of muscle tone. If your patient has dramatically different airflow measurements or sympathetic nervous system response during REM, it is less likely they will benefit from a purely nasal-airflow improvement protocol and more likely MAD will be needed to overcome poor upper airway dilator muscle tone.
Using the myTap to Increase Case Acceptance
If your patient is unsure about wearing a MAD or even the value of treating a diagnosed SRBD, they may be uneasy committing to a custom MAD. After all, CPAP is free to use for most patients for 90 days and can be returned without obligation. A group of prominent researchers/clinicians in Europe are wrapping up a study of myTAP with mouth shield that reveals comparable effectiveness to custom MAD.

Since myTAP is a smaller investment than custom MAD, in my clinic skeptical patients often choose to start with the in-office device to see for themselves. I recommend it frequently to those I’m unsure I will be able to address their whole medical problem using MAD. Simple titration testing using high resolution pulse oximetry, sleep quality index measurements, or even disposable PAT devices gives me objective data the patient and I can use to determine their chosen therapy path.
We charge the patient a cash fee for myTAP trial and apply half of it to any custom MAD out of pocket costs, with them keeping the myTAP as a backup.
The Best Appliance For The Patient...
MAD come in many forms to fit the teeth – hard acrylic, soft liners, printed nylon, thermoformed, metal framework, and heat-and-fit. Each patient can be evaluated for what matches them best. People who have invested in many porcelain restorations, for example, are often more comfortable with a soft liner they feel won’t harm their crowns. Short round teeth with little retention can provide anchorage using acrylic with ball clasps. MAD that do not include rigid connectors between the arches, like Herbst or dorsal designs, needless retention than those that depend on each arch resisting dislodgement as TAP designs do.
Each patient must demonstrate in the office at the delivery day the ability to place and remove their new MAD. Team members must carefully observe this activity and offer coaching or adjustments as needed until the patient has developed confidence in their own abilities.

A Comfortable Breakthough In Appliance Therapy
A breakthrough in fitting custom TAP was realized in 2019 – AccuTherm. Thermacryl, a plant-based, heat-softened material, has been used for decades to achieve a custom fit. Different forms of it are used to make myTAP and morning repositioner devices, but the one that makes clinic life easiest is AccuTherm – a layer of slick ThermAcryl bonded to the shell of the MAD and formed over the teeth. This thin layer can be remolded using heat for precise fit from delivery through any changes to the teeth, such as new restorations. Retention can be altered by heating and placing the device over the teeth repeatedly to lower retention, or by adding ThermAcryl to increase it. Relining with ThermAcryl involves no acrylic taste, chance of locking a reline to the teeth, or extra chair time shaping and polishing the new material. It’s all heat molded and shaped using fingers and small scissors. No smell, hot water is all that is needed, and it can be done an unlimited number of times – perfect for dental patients with a treatment plan that includes several posterior restorations spaced over time.
My position that the best appliance for any patient is the one they will actually use, but I always keep science in mind. The TAP family of devices include the most-studied MAD and those with the best clinical outcomes, supported by more than 20 independent studies. No other devices come close to the scientific validity of the TAP. As dentists strive to maintain and enlarge their ‘place at the table,’ we can overcome some of the resistance in the medical community by supporting our clinical wisdom with valid research-based decision-making.
If you would like to learn more about how to use the myTAP in your dental practice then use the button below to connect with the Airway Management team!
Sources
[1] Hoekema A, Stegenga B, De Bont LG. Efficacy and co-morbidity of oral appliances in the treatment of obstructive sleep apnea-hypopnea: a systematic review. Crit Rev Oral Biol Med 2004;15(3):137-55.
Pancer J, Al-Faifi S, Al-Faifi M, Hoffstein V. Evaluation of Variable Mandibular Advancement Appliance for Treatment of Snoring and Sleep Apnea. Chest 1999;116(6):1511-18.
Skinner MA, Robertson CJ, Kingshott RN, Jones DR, Taylor DR. The efficacy of a mandibular advancement splint in relation to cephalometric variables. Sleep Breath 2002;6(3):115-24.
Vanderveken OM, Devolder A, Marklund M, Boudewyns AN, Braem MJ, Okkerse W, et al. Comparison of a custom-made and a thermoplastic oral appliance for the treatment of mild sleep apnea. Am J Respir Crit Care Med 2008;178(2):197-202.
Hoekema A, Stegenga B, Wijkstra PJ, van der Hoeven JH, Meinesz AF, de Bont LG. Obstructive sleep apnea therapy. J Dent Res 2008;87(9):882-7.
Steve Carstensen DDS has treated sleep apnea and snoring in Bellevue, WA since 1988. He’s the Consultant to the ADA for sleep related breathing disorders, has trained at UCLA’s Mini-Residency in Sleep and is a Diplomate of the American Board of Dental Sleep Medicine. He lectures internationally, directs sleep education at Airway Technologies and the Pankey Institute and is a guest lecturer at Spear Education, University of the Pacific and Louisiana State Dental Schools, in addition to advising several other sleep-related manufacturers. For the AADSM he was a Board Member, Secretary-Treasurer and President-Elect. From 2014 – 2019 he was Editor of Dental Sleep Practice Magazine. In 2019, Quintessence published A Clinician’s Handbook of Dental Sleep Medicine, written with a co-author.