Understanding Obstructive Sleep Apnea: A Silent Culprit Behind Daytime Sleepiness and More
Defining OSA
Are you struggling with excessive daytime sleepiness (EDS) or disrupted sleep and can’t figure out why? You might be one of the 936 million adults1 globally affected by a sleep-related breathing disorder known as Obstructive Sleep Apnea (OSA). OSA2 is a condition marked by a reduction or complete stoppage of airflow due to the relaxation of throat muscles during sleep, leading to the soft tissue at the back of the throat collapsing and obstructing the upper airway.
Individuals with OSA typically experience loud and persistent snoring, punctuated by quiet spells during breath interruptions, followed by choking, snorting, or gasping sounds as breathing restarts.
The Hidden Impact of OSA on Daily Life
OSA doesn’t just steal your good night’s sleep; it can sneak into your daily life in ways you might not realize. Individuals with OSA often experience profound daytime fatigue and sleepiness,3 undermining their productivity,4 concentration, and cognitive functioning.5 This can lead to decreased performance at work or school, increased risk of accidents,6 especially while driving, and can strain personal relationships. Moreover, OSA contributes to emotional disturbances, such as irritability, depression, and anxiety,7,8 stemming from chronic sleep deprivation.

Recognizing the Risk Factors: Could You Be At Risk?
Identifying OSA early is key, and for that, awareness of risk factors is crucial as is understanding gender differences in presentation. In men, risk factors such as higher body mass index (BMI), larger neck circumference, and the overall structure of the upper airway contribute to a higher predisposition to OSA. Men are more likely to exhibit classic symptoms such as loud snoring, observed apneas, and daytime sleepiness.

On the other hand, women may present with more subtle or atypical symptoms such as fatigue, insomnia, mood disturbances, and unrefreshing sleep, which can sometimes lead to underdiagnosis. Hormonal factors and differences in fat distribution also play a role in the risk and presentation of sleep apnea in women. Pre-menopause, women are somewhat protected against OSA, but risk increases with menopause, aligning with changes in hormone levels that affect the airway and fat distribution. Additionally, the clinical presentation in women may be less severe in terms of number of respiratory events per hour, yet the impact on daytime functioning and cardiovascular health remains significant.,9,10
These gender-related differences highlight the need for gender-specific approaches in the diagnosis and treatment of sleep apnea.
The Broader Health Implications of OSA
Getting Diagnosed: The First Step to Recovery
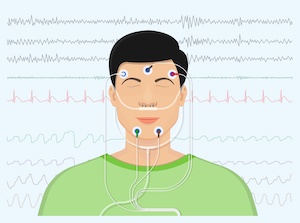
The diagnostic process for OSA typically involves a clinical assessment, potentially followed by either home sleep apnea tests (HSATs) or in-lab polysomnography (PSG). HSATs offer the advantages of convenience, speed, and lower cost, allowing patients to undergo testing in the familiar comfort of their own homes.
Despite these benefits, HSATs may not always capture the full spectrum of sleep disturbances, especially in cases of mild OSA, where their sensitivity can be lower. This limitation underscores the importance of considering a PSG, an in-depth sleep study conducted in a specialized lab, for a more comprehensive evaluation.
In Conclusion
OSA is more than just a sleep disorder; it’s a condition that can permeate every aspect of your life, from your physical health to your daily productivity and emotional wellbeing. If you’re experiencing symptoms like EDS, snoring, or fatigue, don’t wait. Seeking medical attention early can make a world of difference. Remember, a good night’s sleep is not just a luxury; it’s a necessity for a healthy, happy life.
Meet the Author
Dr. Alison Kole, the visionary Founding Medical Director of the Oak Health Sleep Program and CEO of AKMD Consulting, LLC, is a distinguished figure in Sleep, Pulmonary, and Critical Care Medicine. With a track record of integrating advanced sleep diagnostics and treatments, Dr. Kole’s leadership has propelled healthcare practices to new heights in quality and compliance. Dr. Kole’s collaboration with industry partners, including Dental Sleep Medicine and medical equipment vendors, showcases her commitment to pushing the boundaries of medical practice.

References:
1. Benjafield AV, Ayas NT, Eastwood PR, et al. Estimation of the global prevalence and burden of obstructive sleep apnoea: a literature-based analysis. Lancet Respir Med. 2019 Aug;7(8):687-698. doi: 10.1016/S2213-2600(19)30198-5. Epub 2019 Jul 9. PMID: 31300334; PMCID: PMC7007763.
2. OSA Fact Sheet. American Academy of Sleep Medicine. https://aasm.org/resources/factsheets/sleepapnea.pdf.
3. Lal C, Weaver TE, Bae CJ, et al. Excessive Daytime Sleepiness in Obstructive Sleep Apnea. Mechanisms and Clinical Management. Ann Am Thorac Soc. 2021 May;18(5):757-768. doi: 10.1513/AnnalsATS.202006-696FR. PMID: 33621163; PMCID: PMC8086534.
4. Nena E, Steiropoulos P, Constantinidis TC, et al. Work productivity in obstructive sleep apnea patients. J Occup Environ Med. 2010 Jun;52(6):622-5. doi: 10.1097/JOM.0b013e3181e12b05. PMID: 20523238.
5. Wang ML, Wang C, Tuo M, et al. Cognitive Effects of Treating Obstructive Sleep Apnea: A Meta-Analysis of Randomized Controlled Trials. J Alzheimers Dis. 2020;75(3):705-715. doi: 10.3233/JAD-200088. PMID: 32310179.
6. Udholm N, Rex CE, Fuglsang M, et al. Obstructive sleep apnea and road traffic accidents: a Danish nationwide cohort study. Sleep Med. 2022 Aug;96:64-69. doi: 10.1016/j.sleep.2022.04.003. Epub 2022 Apr 13. PMID: 35605348.
7. Pattison E, Tolson J, Barnes M, et al. Improved depressive symptoms, and emotional regulation and reactivity, in individuals with obstructive sleep apnea after short- and long-term CPAP therapy use. Sleep Med. 2023 Nov;111:13-20. doi: 10.1016/j.sleep.2023.08.024. Epub 2023 Sep 1. PMID: 37714031.
8. Gharsalli H, Harizi C, Zaouche R, et al. Prevalence of depression and anxiety in obstructive sleep apnea. Tunis Med. 2022 juillet;100(7):525-533. PMID: 36571741; PMCID: PMC9703910.
9. Lin CM, Davidson TM, Ancoli-Israel S. Gender differences in obstructive sleep apnea and treatment implications. Sleep Med Rev. 2008 Dec;12(6):481-96. doi: 10.1016/j.smrv.2007.11.003. Epub 2008 Oct 31. PMID: 18951050; PMCID: PMC2642982.
10. Geer JH, Hilbert J. Gender Issues in Obstructive Sleep Apnea. Yale J Biol Med. 2021 Sep 30;94(3):487-496. PMID: 34602886; PMCID: PMC8461585.
11. Pack, A.I. Advances in sleep-disordered breathing. Am. J. Respir. Crit. Care Med. 2006, 173, 7–15.
12. Kapur VK, Auckley DH, Chowdhuri S, et al. Clinical Practice Guideline for Diagnostic Testing for Adult Obstructive Sleep Apnea: An American Academy of Sleep Medicine Clinical Practice Guideline. J Clin Sleep Med. 2017 Mar 15;13(3):479-504. doi: 10.5664/jcsm.6506. PMID: 28162150; PMCID: PMC5337595.
13. Setty AR. Underestimation of Sleep Apnea With Home Sleep Apnea Testing Compared to In-Laboratory Sleep Testing. J Clin Sleep Med. 2017 Apr 15;13(4):531-532. doi: 10.5664/jcsm.6534. PMID: 28356176; PMCID: PMC5359328.
14. Caples SM, Anderson WM, Calero K, et al. Use of polysomnography and home sleep apnea tests for the longitudinal management of obstructive sleep apnea in adults: an American Academy of Sleep Medicine clinical guidance statement. J Clin Sleep Med. 2021 Jun 1;17(6):1287-1293. doi: 10.5664/jcsm.9240. PMID: 33704050; PMCID: PMC8314660.