By Brittny Sciarra-Murphy, RDH
Orofacial myofunctional therapy is not a new therapy, it dates back over a century ago when Dr. Alfred Rogers first spoke about the effects of the musculature of the mouth. In 1918, Dr. Alfred Rogers, also known as the Father of Myofunctional therapy in orthodontics, developed a series of exercises for each facial muscle and stated that he believed “the culture of the muscles of mastication and the so-called muscles of expression is of paramount importance when considered in relation to their influence upon the developing bony structure beneath them.
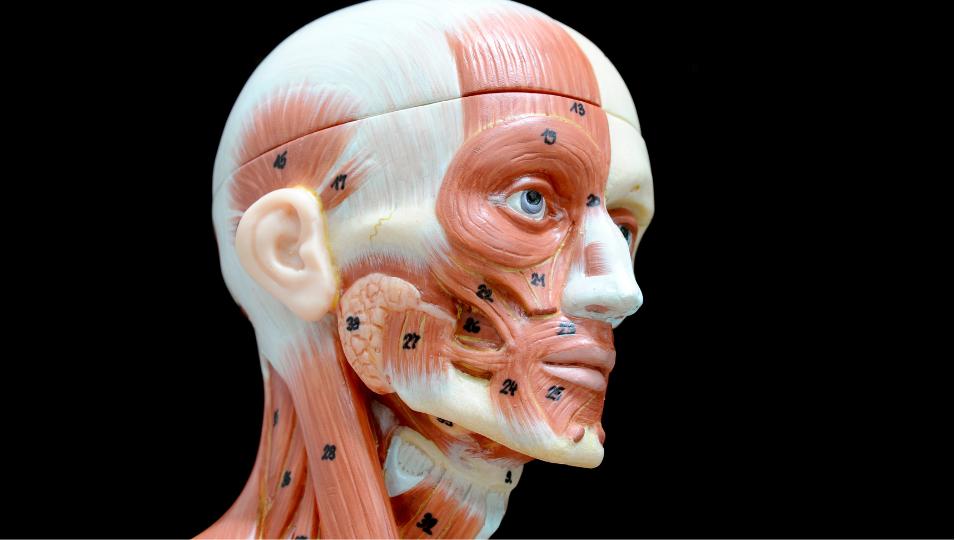
The Role and Applications of Myofunctional Therapy in Oral and Facial Health
Myofunctional therapy is the neuromuscular re-education and strengthening of the muscles of the face, lips, tongue, and pharyngeal airway. According to Sandra Holtzman, MS, CCC-SLP, QOM® of Neohealth Services, orofacial myology, another name for orofacial myofunctional therapy, is defined as the study and treatment of oral and facial muscles as they relate to speech, dentition, chewing/bolus collection, swallowing, and overall mental and physical health.2 Myofunctional therapy can be a key component in the treatment of sleep-related breathing disorders for adults and children, malocclusion and orthodontic stability, temporomandibular joint dysfunction, orthognathic jaw surgery, and can help prevent health problems into adulthood by guiding the child through craniofacial growth and development. Symptoms of orofacial myofunctional disorders include, but are not limited to:

- Mouth breathing
- Prolonged non-nutritive sucking habits (thumb, finger, pacifier)
- Open mouth rest posture
- Forward, interdental, lateral, or low tongue rest posture
- Tongue thrust
- Restricted lingual frenulum
The main goal of a myofunctional therapy program is to restore correct oral rest posture. Correct oral rest posture includes:
- exclusive nasal breathing, all day and all night
- lip seal, all day and all night
- tip, middle, and back of tongue lightly suctioned to the palate all day and all night
- back teeth slightly apart
The Importance of Proper Tongue and Lip Resting Positions for Oral Health
At rest, your tongue should be resting on the palate, and your lips should always be closed. Say the letter ‘N’. Feel where the tip of your tongue hits right behind your upper front teeth? This should be the natural resting position of the anterior tongue. The posterior body of the tongue should be lightly suctioned in the palate as well. Unfortunately, for a majority of my patients, this is not where their tongue rests. It may be on the floor of their mouth or between their teeth. Somewhere along the way, something went wrong. We are born obligate nasal breathers. Our tongue should act as a natural palate expander resting on the roof of our mouth. If in the correct position, our upper jaw will develop a “U” shaped arch allowing room for our adult teeth to come in straight, versus a “V” shaped or omega-shaped arch which would be high and narrow causing constriction and malocclusion.

It is when our tongue posture drops, we generally tend to begin breathing through the mouth. Try it yourself, suction your tongue into the roof of your mouth and open wide. Try to breathe through your mouth. It is physically impossible.
Building Sustainable Habits and Awareness through Myofunctional Therapy
Some say myofunctional therapy is like physical therapy for your mouth. My colleague likens myofunctional therapy to personal training, and I love this analogy even more. You can work with your personal trainer 3x a week, but if you leave the gym and your next stop is the drive-through line at McDonald’s, you are not creating sustainable lifestyle changes.

Similarly, in order for us to habituate and generalize new patterns learned throughout the myofunctional therapy program, we must learn to create an overall awareness of how our muscles are functioning. For example, every time you start your car, check:
- Where is my tongue?
- Where are my lips?
- How am I breathing?
For a child, you can have them place stickers in areas around the house where they visit often. When they see those stickers that aren’t usually there, that will trigger them to check in on their oral rest posture.

As a myofunctional therapist, we teach facial and tongue exercises and behavior modification techniques to promote optimal breathing and oral rest posture. We often get referrals for a tongue thrust swallowing pattern. However, the tongue thrust is a symptom, not a diagnosis. An incorrect swallowing pattern will be addressed through optimizing the correct oral rest posture. I always tell my patients:
“Your orofacial muscles are like any other muscle in your body- if you don’t use it, you lose it!”
Finding the Root of the Problem
As a myofunctional therapist, we must find the root cause of the problem. Why did somebody begin to mouth breathe? Do they have enlarged tonsils or adenoids? Do they have a deviated septum or enlarged turbinates? Do they have a tethered oral tissue such as a tongue-tie that is tethering their tongue to the floor of their mouth? In that aspect, myofunctional therapists are like detectives.
However, we can’t do it alone. We must work as an interdisciplinary team for optimal patient outcomes. Collaboration is key. Myofunctional therapists are an important piece of the puzzle, but they are not the only answer. For example, if I have a patient who comes to me with a high, narrow arch and a chronic mouth breathing habit, I can’t just enroll them in a myofunctional therapy program and hope for the best. I would recommend they see an ENT provider who can assess the patency of their airway and a dental provider who can evaluate their craniofacial development and treat as necessary.
Myofunctional therapy is gaining popularity rapidly. Not only are more healthcare professionals becoming interested, but there is an increased awareness in the general public. As dental professionals, we are at an advantage, spending the majority of our time in the oral cavity. The oral cavity is the gateway to overall health.
That coupled with our patient’s medical history can spark a conversation with our patients that can truly transform their lives. In the next article, we will discuss how we can easily observe and assess our patients while they are not only in our operatories, but even in the waiting room. Be on the forefront of airway health, begin working today with a myofunctional therapist in your community or find one who can treat your patients virtually!
Meet the Author:
Brittny Sciarra-Murphy, RDH, BS, MAS™, COM® is a registered dental hygienist, myofunctional therapist, Buteyko Breathing educator, leader, speaker, and mentor. Brittny is the founder of CT Orofacial Myology and co-founder of MyoAir. Brittny teaches other registered dental hygienists to become myofunctional therapists through the Team Myo program at Airway Health Solutions. She is also the face behind the podcast “I Spy with My Myo Eye” available on all major podcast platforms.